
Over the past few weeks we have been speaking to all those involved with providing the cervical screening service to over 4 million participants a year in England.
Throughout this blog post I'm going to avoid using the pronoun her or women because anyone with a cervix needs to be screened - that includes trans men.
We've been speaking to GP practices who book appointments, sample takers who perform the test, labs that analyse the samples and the back office that provide the complex IT infrastructure that is the backbone of the screening service. We are trying to make sense of all the interactions and information exchanges that happen from start to finish.
The start of the service begins with making a list of eligible participants to invite for cervical screening and includes obtaining results, sending results back to participants and setting their new call back date.
Breaking down the service
To explain the service in simple terms, this is what happens:
- Identify those in the population who are ready to be screened and eligible (if you are within age, have a cervix, are not pregnant and are not going through cervical cancer treatments)
- Send eligible participants an invitation letter to get screened
- The participant books an appointment with a sample taker (usually a practice nurse)
- A sample is taken by a sample taker or practice nurse
- The sample is sent to a lab to test for HPV and abnormal cells
- The labs share the results
- Results are sent to participants
- The next test date is set depending on the results of the sample
- Treatment is arranged for anyone with significantly abnormal cell (these are not cancer cells but, over time, could become cancer cells if not treated)
- When this simple treatment has finished, the next test date is set
Mapping the service tells us who is doing what, what are their tasks and how they are communicating information to other parts of the service.
We build maps based on the information we gain from our research. We conducted our research by not only asking service providers what they are doing but also watching them in their environment. This is important because everyone does something different and we learn from all those differences.
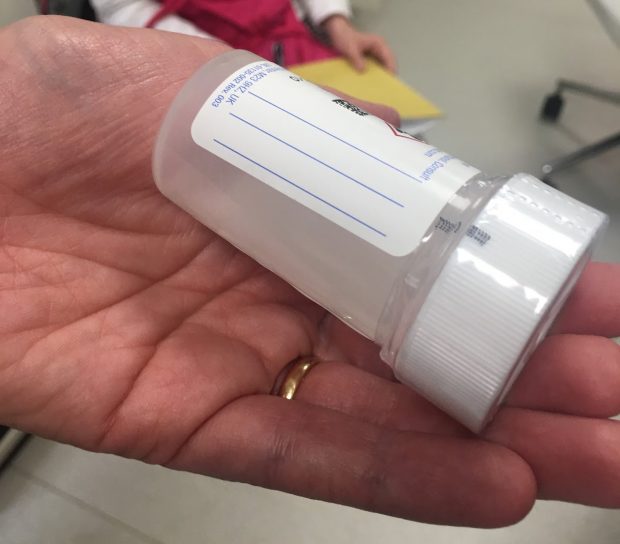
We also pay close attention to the small details, such as the size of the label that sample takers write information on or the many screens and workarounds service support have to operate to get their work done.
All these little things are what makes conducting research so special in someone’s environment. We want to not only learn what they are doing but also how they are doing it.
All the information that we gather is shared with the team and slowly we start to put together the story of each person in the service process.
Visualising the tasks and experiences
To make sense of what is happening, we use online whiteboards to help us see the whole picture. We map the journey and add in bits like problems, needs, opportunities and quotes to build the experiences each service provider goes through.
We start small and then fill in the blanks using more research. Each research session helps us to understand where we can improve the service. What is causing issues towards the end of the process? If we fix that part of the journey, will it help remove some burden towards the end?
This is what I'm looking for. As the senior service designer on this project I'm always on the lookout for cause and effect.
I love maps because they help the whole team visualise the story so we as a group can make sense of it all and think of ways to fix the breaks.
We will be continuing our research and at the end of our discovery we will be able to come out with a few ideas to make the service more efficient for not only the participants who are screened, but all the people involved with making it happen.
If you’d like to be involved with our research please contact digitalresearch@nhsx.nhs.uk
1 comment
Comment by Ben Rusholme posted on
Where laboratories are looking for HPV in samples first, participants who have had the HPV vaccine may ask why they need cervical screening. It would be great to get some clarity on this in the service.